Transforming Healthcare Through Cost & Quality of Care Analytics


The payer industry for Medicare is changing. Medpac’s June 2025 medicare report to the Congress mentions reducing beneficiary/patient cost sharing for outpatient services at critical access hospitals as one of the key considerations.
This is because costs are going up and the quality of care is becoming harder to maintain. Many people on Medicare have chronic conditions and need more support. At the same time, they want better care without higher costs. Regulators like CMS are also asking for more transparency and better results from payers. To keep up with these requirements, payers need smart tools. These tools must help manage costs while also improving patient care and meeting strict rules.
Tools like Innovaccer’s Cost & Quality of Care Analytics can help payers navigate different requirements. These tools help payers make better decisions using data, improve patient health and save money, among other things.
What is Innovaccer’s Cost and Quality of Care Analytics Tool?
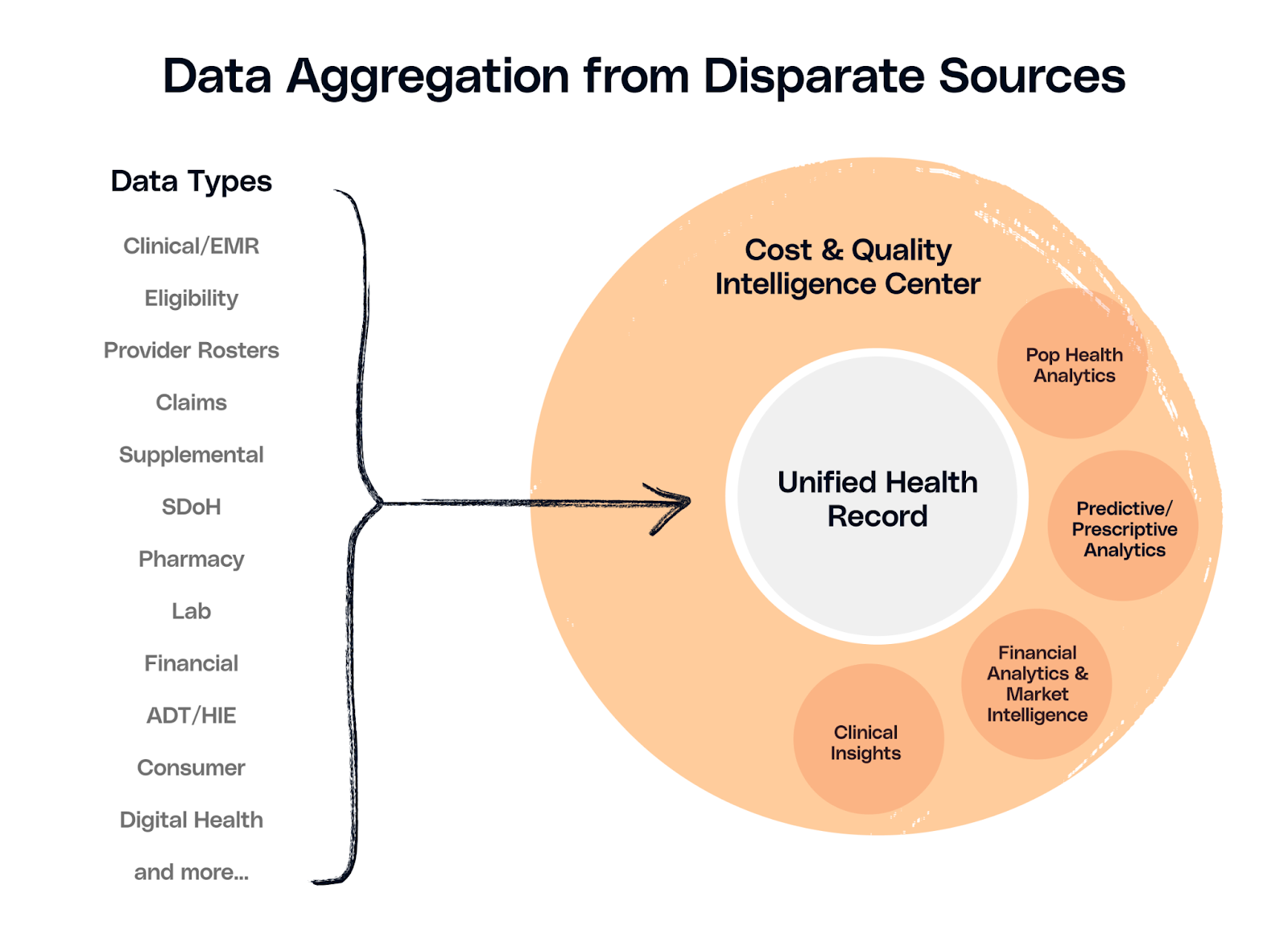
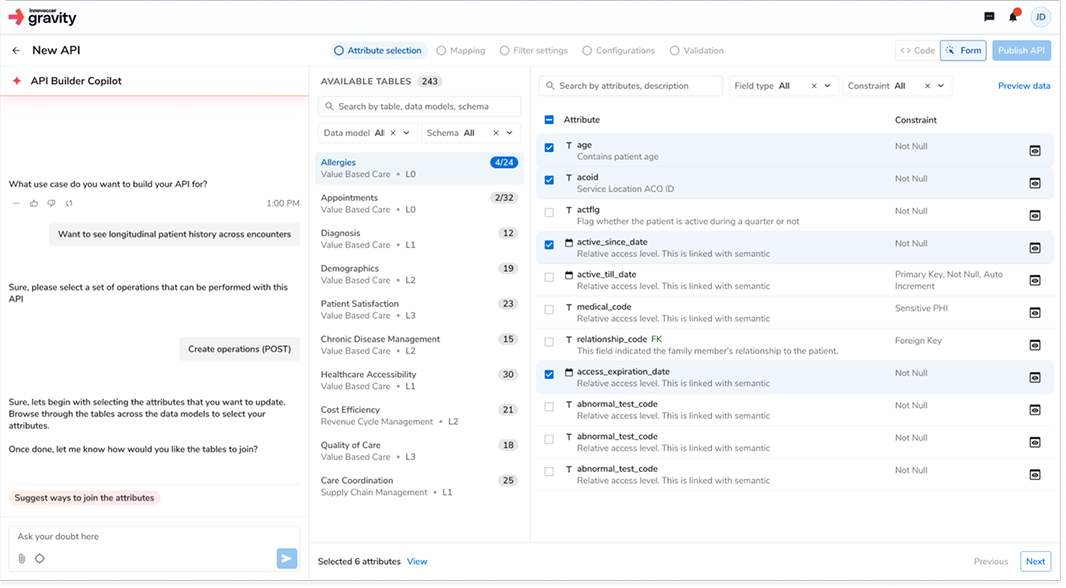
Innovaccer’s Cost & Quality of Care Analytics tool looks at healthcare data in a new way. This tool examines how medical spending relates to patient outcomes across all healthcare entities.
For Medicare payers, having timely access to critical data is important to control member plans better and manage costs. Critical data includes ADT feeds, prescription claims, and lab results. Platforms like Innovaccer’s Cost & Quality of Care Analytics suite combine deep expertise in healthcare data with a 360-degree view of each patient. This is especially important in Medicare, where managing chronic conditions and care transitions can significantly impact CMS Star Ratings and total cost of care for payers.
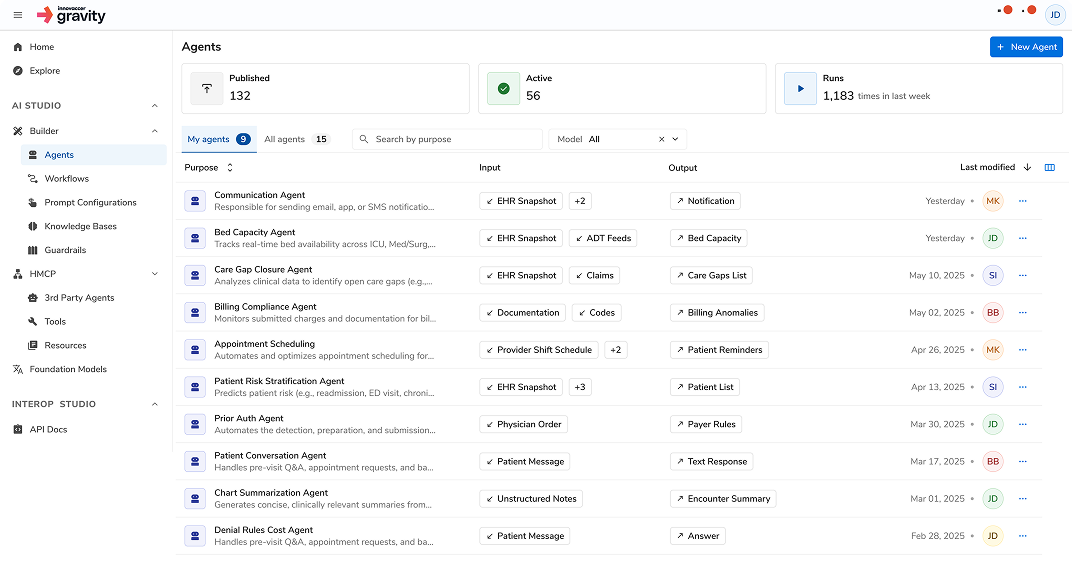
Innovaccer's solution give payers the tools they need, with key features including:
| Feature | Description | Business Impact |
|---|---|---|
| Performance Dashboards | Shows cost and quality of care by line of business, geography, provider, and network | Enables drilled-down analysis for targeted interventions |
| Cost Breakdowns | Detailed analysis by category, episode, diagnosis codes, and care locations | Identifies specific cost drivers and savings opportunities |
| Custom Comparisons | Compares against past performance and industry benchmarks | Tracks improvement and competitive positioning |
| Machine Learning Insights | AI-powered identification of cost drivers and savings opportunities | Proactively identifies issues before they escalate |
| Unified Analytics | Integrated groupers and predictive models | Provides a comprehensive view across all payer functions |
The platform applies machine learning and predictive analytics to detect risks in advance and recommend the optimal course of action. Insights are easily shared across teams to ensure everyone in the organization is operating from the integrated data-driven playbook.
Why Cost and Quality Integration is Important for Payers
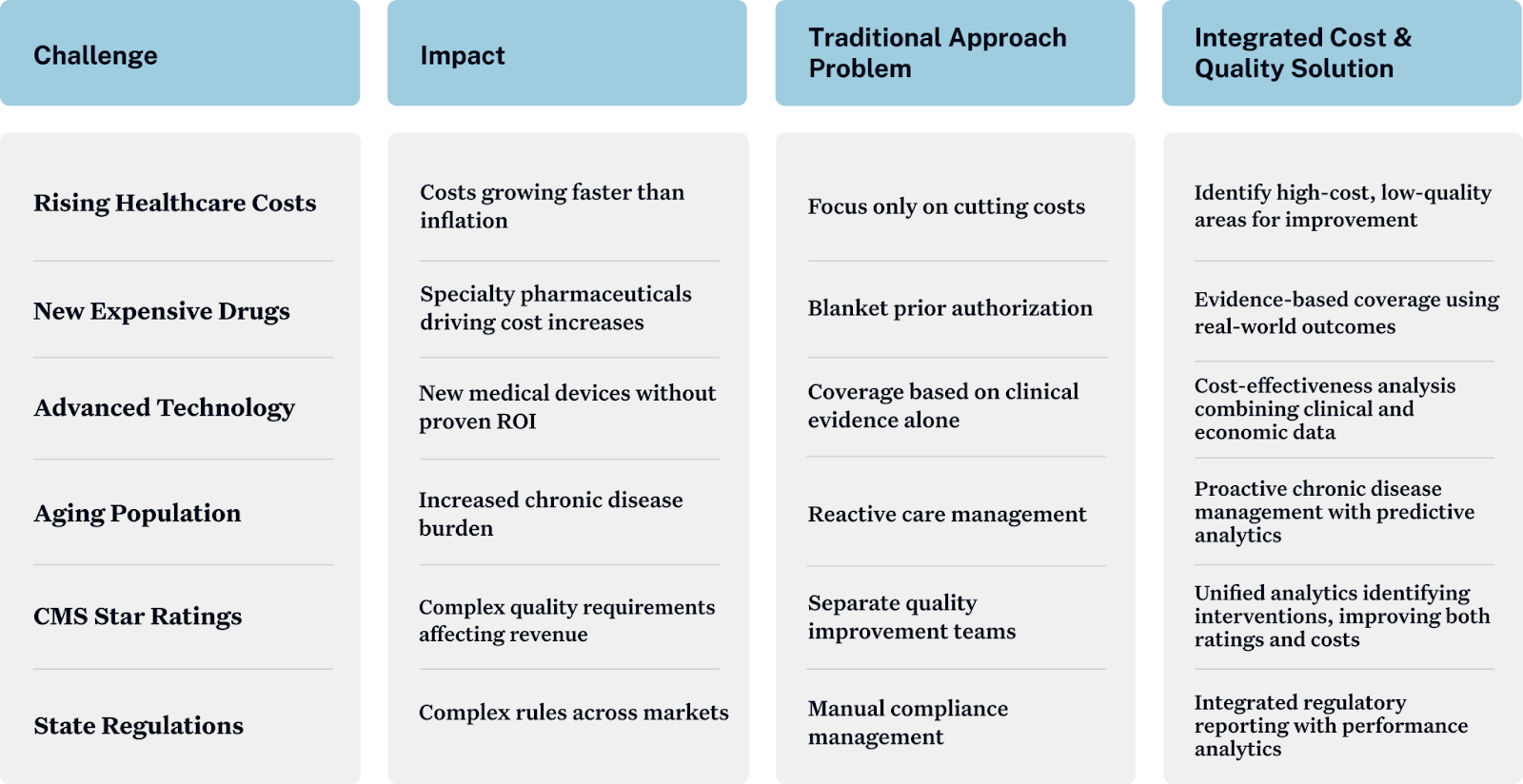
Since payers are confronted with increasing costs and more stringent regulation while patients increasingly demand improved care and online convenience, cost and quality cannot be managed separately anymore. Progressive payers must bridge the two, deriving value from initiatives such as prevention and chronic care. This enhances patient outcomes, lowers cost, and creates a more sustainable healthcare model.
Challenge-Solution Matrix
Value Opportunities from Integration
Integrated approaches that connect cost and quality don't merely enhance care, they realize quantifiable value. By coordinating financial and clinical objectives, payers are able to identify high-impact opportunities that eliminate waste, enhance outcomes, and increase patient satisfaction. Some value levers that have targeted investment leading to better health as well as better financial performance are illustrated below:
- Preventive Care Programs: Invest in higher screening and wellness expenses to lower complications related to chronic disease, realizing improvement in preventive care use.
- Care Coordination: Utilize care managers and technology investments to lower readmissions and care gaps, realizing decrease in care transition problems.
- Chronic Disease Management: Fund costs of diabetes and heart disease programs to lower emergency visits and complications, providing improved patient outcomes at lower total costs.
- Provider Network Enhancements: Make an investment in network growth and contracting to have higher quality providers and improved outcomes, enhancing member satisfaction and cost effectiveness.
Building a Data-Driven Culture for Payers
Creating lasting change involves developing an analytics culture across the payer organization. That means developing data-driven decision-making processes in all functions. From medical management to network operations to patient services.
Leadership commitment is paramount. Payer executives need to champion analytics efforts and deploy needed resources. When leaders repeatedly use analytics to inform their decisions, it demonstrates to the organization that this approach is valued.
Essential features of a data driven culture include:
- Cross-functional data analytics teams with medical, actuarial, quality and operating skills
- Processes for regular data review that drive planning
- Analytical training programs that develop capabilities
- Incentive performance metrics that encourage data-driven decisions
- Investments in technology in support of analytics self-service
The Advantage and the Future for Payers
Payer organizations that achieve successful comprehensive analytics platforms reap considerable competitive benefits. Top solutions offer real-time access to pertinent data such as ADT, prescription claims, lab results, and other vital details. The analytical prowess of processing healthcare information, along with end-to-end patient views and machine learning analytics, develops considerable operational benefits.
Cost & Quality of Care Analytics is not just technology. It's a paradigm change in the way payer organizations discharge their mission. Those payers who are able to implement these capabilities effectively will be well on their way to thriving in a more competitive healthcare landscape.
This path to successful analytics is not easy though. It takes dedication, investment, and perseverance. But the potential payoff makes this journey worthwhile. They are better patient outcomes, increased financial performance, more robust provider relations, and lasting competitive advantage.
As healthcare becomes increasingly advanced, payer organizations embracing analytics will drive the change. They will produce a more effective, efficient, and patient-focused healthcare system. The moment to start this process is now. Payer organizations are under increasing pressure to prove both clinical stewardship and financial results.
The future of healthcare rests upon payers' capacity to manage costs while improving quality. With advanced analytics, payer organizations can strike the right balance. They can accomplish their core mission of providing access to quality, affordable healthcare for their patients. This is not merely an operational enhancement. It's a strategic imperative that will determine the next generation of winning payer organizations.
Ready to transform your healthcare system with cost and quality of care analytics? Book a demo now.

.png)



.png)




