Integrating AI into Prior Authorization: From Fragmentation to Flow


Prior authorization has become healthcare's most contentious administrative process, a system originally designed to control costs and ensure appropriate care that now paradoxically drives up expenses while delaying critical treatments. Physicians and staff consistently report spending substantial portions of their workweek navigating prior authorization requirements, with the vast majority citing delays in patient care and significant contributions to professional burnout. Physicians report that prior authorization frequently results in patients abandoning recommended treatments, creating a system where the administrative cure has become worse than the disease it was meant to address.
Meanwhile, payers continue expanding these requirements, Medicare is introducing prior authorization to traditional fee-for-service through programs like the WISeR model, which aims to reduce wasteful spending on low-value services through technology-enhanced review processes. A system designed to prevent waste is itself generating enormous waste, with healthcare organizations losing millions annually to denial management processes that could be largely automated.
Yet within this crisis lies unprecedented opportunity. The convergence of AI, policy reform, and industry recognition of prior authorization's failures is creating a perfect storm for transformation. Just as AI has proven capable of automating complex healthcare administrative workflows, the same technologies can reshape prior authorization from a reactive, manual burden into a proactive, intelligent system. Policy initiatives like CMS's push for interoperability and API-driven workflows, combined with AI's ability to understand complex medical documentation and payer policies, offer a path toward prior authorization that actually serves its intended purpose: ensuring appropriate care while minimizing administrative friction. The question is no longer whether this transformation will happen, but how quickly we can implement solutions that turn prior authorization from healthcare's greatest administrative pain point into a seamless, value-adding process.
How it Works:
Prior authorization (PA) remains a largely manual process in most health systems. When a physician orders a medication, test, or procedure that may require insurer approval, dedicated staff must first verify the patient's insurance status and determine if authorization is needed under their specific plan. This involves navigating multiple payer websites, portals, and often making phone calls to various departments. If PA is required, staff must consult the insurer's medical necessity guidelines; each payer and plan maintains distinct requirements, then gather necessary clinical documentation from the patient's record, including diagnoses, physician notes, imaging results, and laboratory findings. The PA request is submitted through the insurer's web portal, phone or by fax.The waiting period for an initial determination ranges from one day to weeks, during which staff frequently follow up to manually check the status. The insurer will approve the request, ask for additional information, or deny coverage. Denials or requests for more information require staff response and may involve peer-to-peer discussions between physicians and the insurer's medical reviewers, potentially triggering appeals that can extend the process from days to months.Throughout this workflow, the physician's staff bears responsibility for navigating each payer's unique requirements and ensuring resolution, creating substantial administrative burden while patients wait for necessary care.
Problem Areas within a Manual Prior Authorization Workflow:
Inefficient, Fragmented Workflows
The prior authorization process remains largely manual and disconnected from core clinical systems. Staff must log into multiple payer portals, fax forms, upload documents to benefits manager platforms, and make phone calls to verify requirements or check status. These steps are performed outside the EHR with little standardization across payers or automation in submission workflows. Only 35% of prior authorizations are completed using fully electronic transactions, while the vast majority rely on manual methods like phone, fax and payer portals. A phone call to a payer to ask for a clarification can keep the staff on hold for 15-20 minutes before they even get connected with someone. This fragmentation leads to duplicated effort, lost productivity, and longer turnaround times for both routine and complex cases.
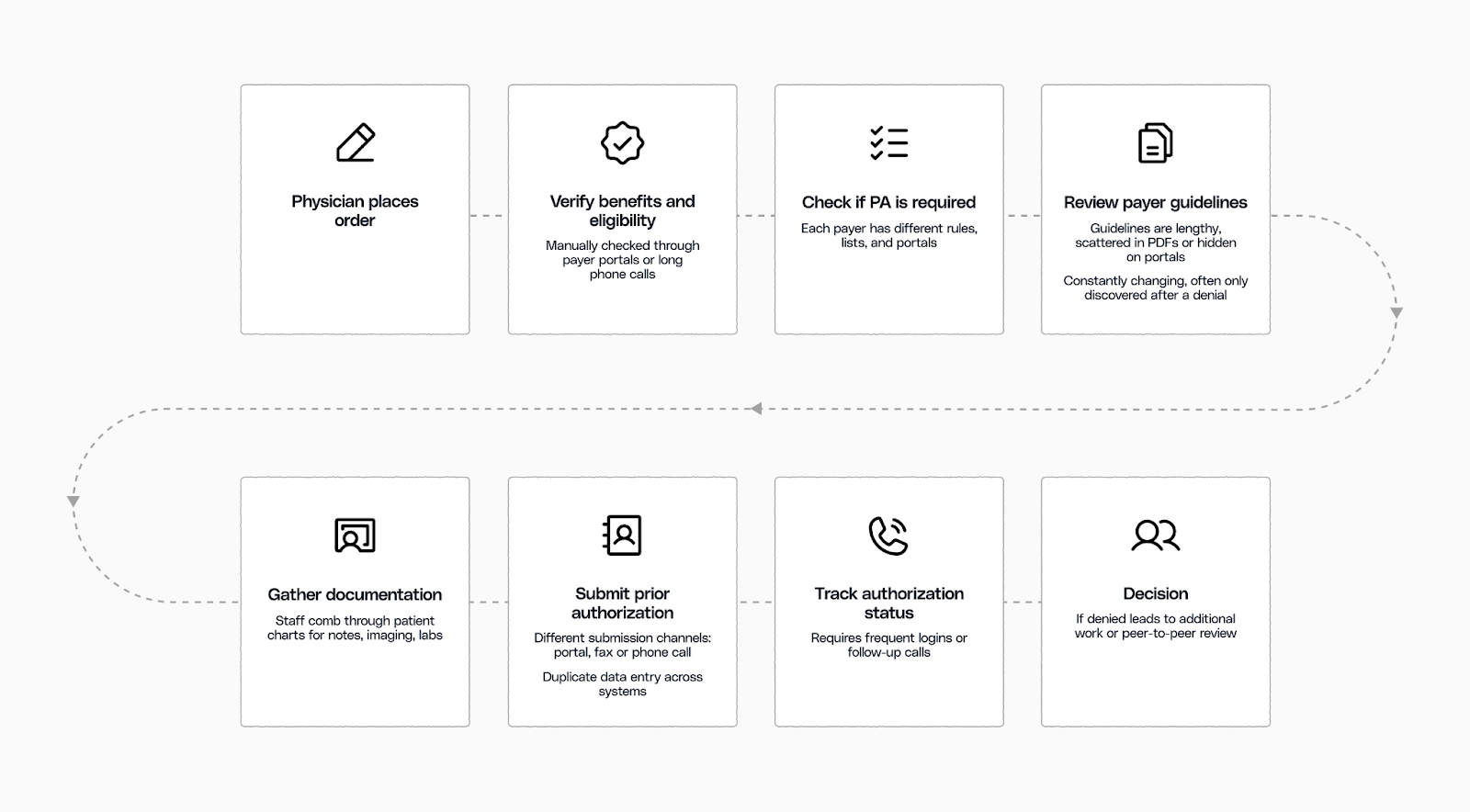
Payer Variability Is a Universal Headache
With hundreds of payers, thousands of plan variations, and constantly shifting requirements, prior authorization staff face an impossible navigation challenge. Every insurer operates with its own rules, portals, forms, and medical necessity criteria, none of which are standardized across the industry. Medical necessity guidelines change frequently and are often buried in lengthy PDFs or scattered across third-party portals, with no notification system to alert providers of updates. UnitedHealthcare's radiology guidelines alone exceed 3,000 pages, while other payers may have different requirements for the same procedure. Even within the same payer, requirements can vary dramatically by plan, region, or line of business. Compounding this complexity is determining where to submit each request. Submission channels may vary between the payer's own portal, a clearinghouse, or a delegated benefit manager often depending on the service type, geographic region, or specific contract terms. This variability leads to wasted time searching for the correct channel or submitting through the wrong one entirely, adding avoidable delays to an already cumbersome process.
Clinical Documentation Is a Major Point of Friction
Gathering and preparing clinical documentation to support medical necessity guidelines is one of the most resource-intensive and error-prone steps in the prior authorization process. Staff must navigate lengthy payer guidelines and match them against the patient's chart. For complex services like infusions or advanced imaging, this requires detailed reviews of progress notes, labs, imaging reports, and past treatments. Because EHRs and payer systems are not integrated, teams must manually extract and re-enter clinical data into prior authorization portals or questionnaires. Denials citing "lack of medical necessity" are common and often reflect gaps in not only being up to date on the guidelines but also the challenge of finding and pulling together the appropriate clinical documentation from the patient chart.
Denials and Appeals Drive Avoidable Rework
Prior authorization denials are common,and often preventable. In 2023, Medicare Advantage plans denied 3.2 million requests, yet over 81% of appealed cases were later approved. These reversals point to errors or overly strict reviews that create unnecessary delays. Despite this, fewer than 12% of denials are appealed, due to the time and effort required. Each appeal adds administrative work, extends care timelines, and increases staff fatigue. When denials go unchallenged, patients may forgo needed treatment, and health systems risk lost revenue for services that should have been covered.
An AI-First Solution
These systemic problems require a fundamentally different approach, one that can handle complexity - given the variety in clinical documentation, learn from patterns, and adapt to constant change.
Artificial intelligence advancements post the advent of transformers, particularly large language models and AI agents, offer the first viable path and a unique opportunity to transform prior authorization from a manual burden into an intelligent, automated process. AI agents are sophisticated software orchestrations that can understand natural language, analyze complex documents, make decisions based on rules and patterns, and interact with multiple data sources and systems autonomously, exactly the capabilities needed to navigate prior authorization's fragmented landscape.

Unified Workflow Integration
Instead of forcing staff to toggle between payer portals, changing policy documents, and phone trees, our system consolidates all activity into one interface integrated within the EHR. Our AI agents initiate eligibility checks, pull plan-specific PA rules, surface whether authorization is needed, populate forms using patients data and submit authorization requests. These agents are built to handle the full range of payer connectivity, whether through modern APIs, payer portals, or fallback channels like phone and fax, ensuring every request can move forward regardless of how advanced or limited the payer's infrastructure is.
While the system automates the most repetitive and time-consuming tasks, a human remains in the loop for final review—providing oversight, making judgment calls when needed, and ensuring confidence before submission. This flexibility allows teams to operate in a single, consistent workflow while the underlying system handles the complexity and nuances.
Intelligent Knowledge Management
To address the nuances seen across payer guidelines, we built an AI-powered knowledge base that serves as the engine behind every prior authorization decision. It ingests the most up-to-date medical necessity guidelines, authorization criteria, and policy documentation across payers, plans and lines of business. It not only keeps track of multiple versions of policies, but also mines it to convert them into a logical decision tree for digital evaluation.
Automated Clinical Documentation Review
As PA requests arise, a swarm of AI agents get to work to get an accurate and fast decision on the prior auth. While one agent identifies the relevant guidelines and decision tree from the knowledge base, another performs a medical necessity review by analyzing the patient's clinical records in the EMR against those criteria. A third agent extracts relevant semi-structured data such as progress notes, imaging results, prior treatments, and lab values and compares it to the specific documentation requirements set by the payer. The system then highlights which clinical elements satisfy the criteria and flags any missing or insufficient information.
This ensures that every submission includes the necessary evidence to support approval, without requiring staff to manually sift through the chart or interpret lengthy policy documents. By clearly identifying what must be shared with the payer-and why-the system helps teams submit complete, defensible requests the first time.
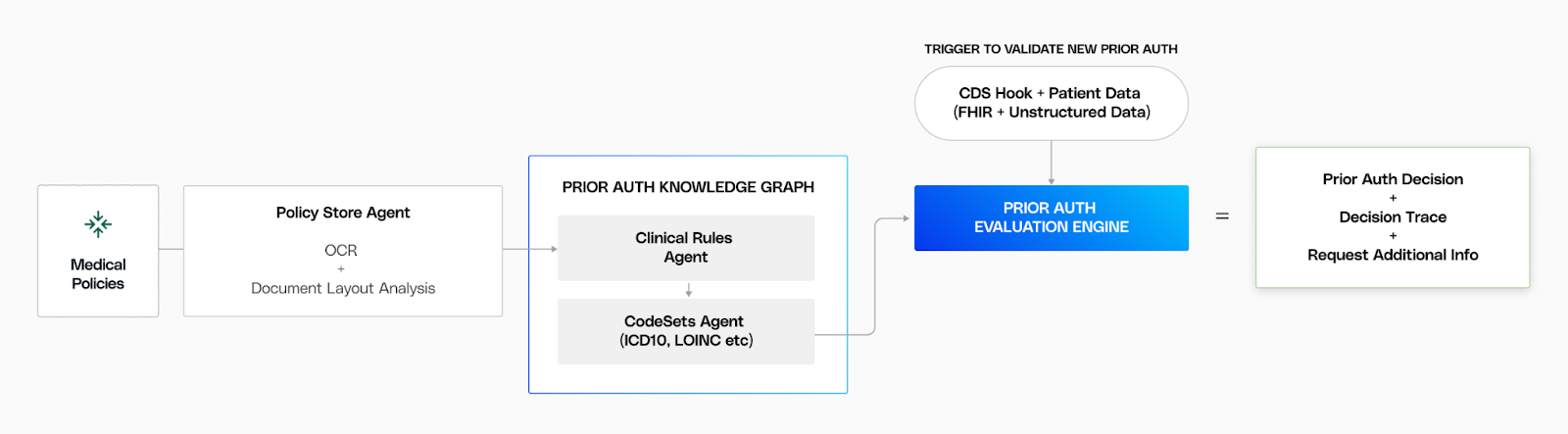
Continuous Learning and Optimization
Finally, we close the loop on denials through continuous learning. Every payer response, whether a pending, approval, denial, or appeal outcome, feeds back into the engine to refine and update the logic. This ensures our system reflects not just what payers state in their policies, but what they actually do in practice.
The system surfaces patterns that previously led to rework, alerting prior authorization staff to potential issues before submission. Over time, these insights refine our recommendations, reducing unnecessary appeals and increasing first-pass approval rates. When appeals are necessary, the system automatically pre-packages the required documentation according to specific payer rules, minimizing staff effort and accelerating resolution.
The Result
With the power of AI, Innovaccer’s prior auth solution doesn't just automate prior authorization, it demystifies the entire black - making it understandable, predictable, and efficient. By delivering clarity where there was once complexity, we enable teams to move faster, reduce denials, and restore focus to patient care.

.png)



.png)




