End-to-End Quality Management: Driving Consistent Results for Health Plans


Quality management in healthcare has evolved beyond simple compliance. For payers, it's now a mission-critical function that directly impacts everything from financial performance to member satisfaction. In today's value-based care landscape, a strategic investment in quality management is a powerful lever to lower medical costs and boost member retention.
Consider a health plan struggling with its STAR ratings and avoidable costs. By deploying a robust quality management solution, they can streamline gap closure across both providers and members. This not only leads to more closed care gaps but also a significant reduction in preventable emergency room visits, ultimately improving financial performance and the member experience.
Making quality management a strategic priority isn't just a good idea—it's essential for long-term success.
The Rising Pressure: Navigating Regulatory and Performance Demands
The stakes for payers are higher than ever. The Centers for Medicare & Medicaid Services (CMS) is sharpening its focus on accountability, making it more challenging for plans to achieve top-tier scores. The latest updates to the Medicare Advantage (MA) and Part D Star Ratings program require consistent, system-wide improvements across a broader range of measures just to maintain a 4-star rating or higher.
CMS is also pushing for a future defined by real-time data sharing and digital quality measurement through the Interoperability and Patient Access Final Rule. Simultaneously, organizations like the National Committee for Quality Assurance (NCQA) are continuously raising the bar for care quality and member experience. Their HEDIS® measures, which are the gold standard for evaluating health plan performance, are constantly evolving.
This combination of rising performance benchmarks and compliance requirements makes a modern quality management strategy non-negotiable for payers who want to stay compliant and competitive.
Why Quality Management is a Strategic Advantage
Moving beyond compliance, a strong quality management program delivers tangible benefits to health plans:
- Higher STAR Ratings and Quality Measures: By embedding quality into daily workflows, health plans can proactively improve key metrics that lead to higher STAR ratings and financial incentives.
- Reduced Avoidable Costs: Proactive care management helps health plans detect and close care gaps sooner, leading to timely treatments that prevent costly hospitalizations and ED visits.
- Empowered Provider Networks: Payers can play a pivotal role in enabling high-quality care. By sharing real-time data and actionable insights, they can help providers focus on patient outcomes rather than administrative tasks.
- Improved Member Satisfaction: A member-centric approach to quality, including personalized reminders and follow-ups, builds trust and boosts satisfaction and engagement.
- Clearer Visibility and Accountability: A centralized quality tracking system allows payers to monitor progress across their entire network and member population, enabling faster decision-making and more targeted interventions.
The Challenges of Today’s Quality Management
Despite its importance, quality management remains a complex and resource-intensive process for most payers. Here’s why:
- Fragmented and stale data: Health plans often rely on disparate systems and outdated data exchanges. Without timely, accurate member and provider data, closing care gaps becomes inefficient and reactive.
- Lack of centralized insights: The absence of a unified dashboard makes it difficult for payers and providers to see quality metrics and performance data in one place. This delays a clear understanding of shortcomings and the ability to take the right action.

- Manual chart reviews: Payers are still spending countless hours on manual chart reviews and chases. This is resource-intensive and slows down everything from quality reporting to gap closure efforts.
Innovaccer’s End-to-End Quality Management Solutions
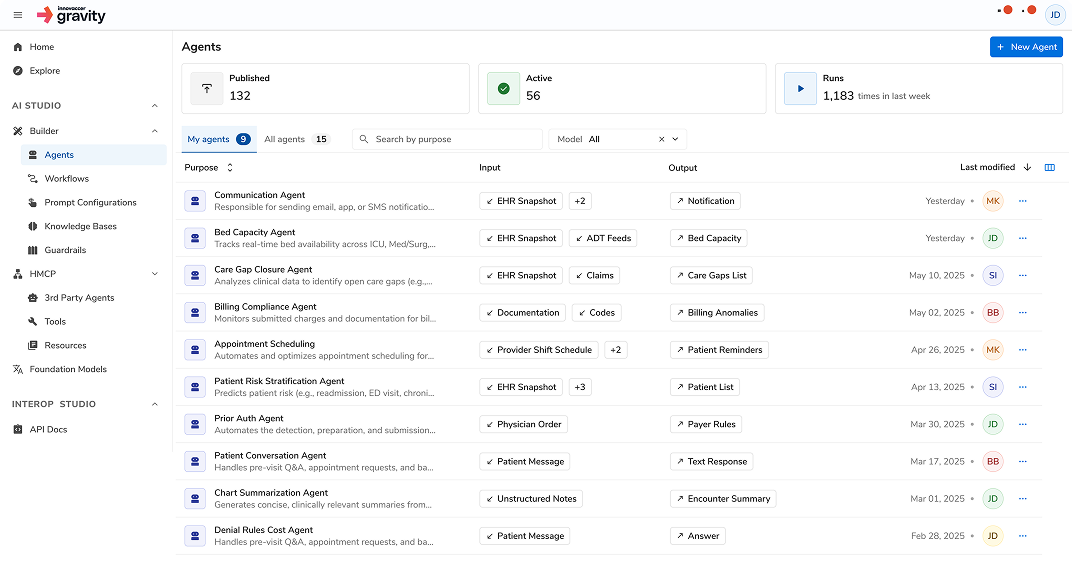
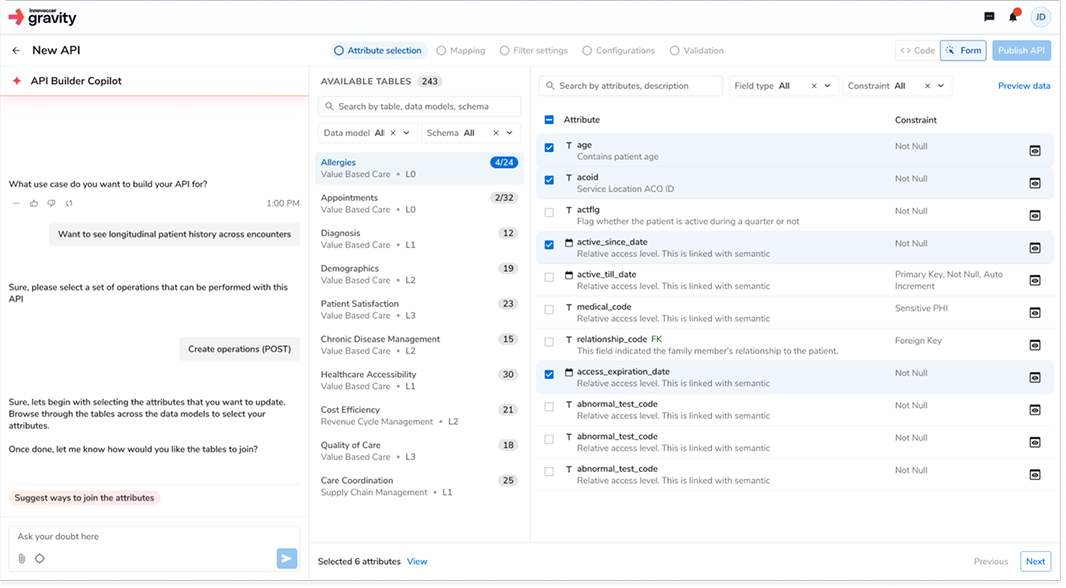
Innovaccer empowers health plans to overcome these challenges with a suite of AI-powered solutions that deliver real-time insights and coordinated workflows. Our platform and solutions help you close care gaps, boost STAR ratings, and strengthen provider and member relationships.
The Quality Management Analytics Engine
Our NCQA-certified Quality Analytics Engine automates and optimizes your entire quality management processes. By continuously processing clinical and claims data, it provides real-time visibility into HEDIS and STAR ratings, helping your health plan stay ahead of compliance deadlines and performance benchmarks.
This platform replaces fragmented, manual processes with an AI-powered, interoperable system that eliminates redundant chart reviews. Its centralized dashboards give stakeholders a clear, real-time view of quality performance, allowing teams to make actionable insights to prioritize interventions and prepare submissions faster.
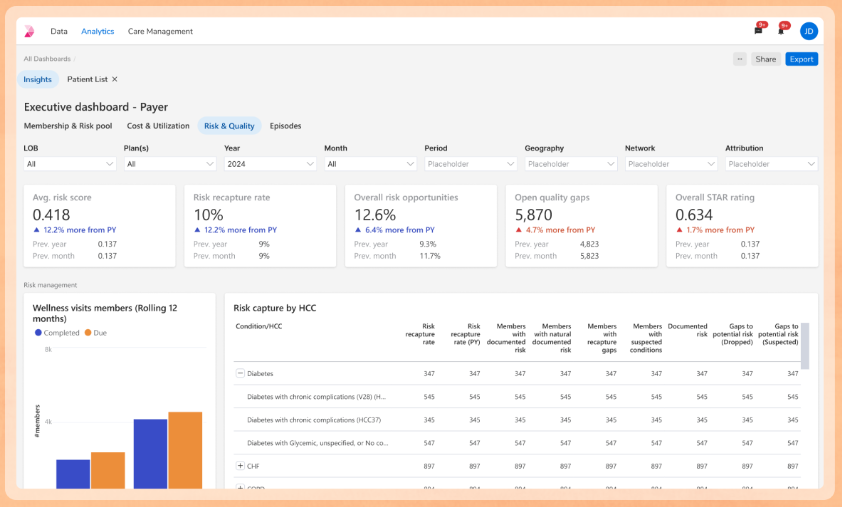
Interactive Dashboards with Near Real-Time Reporting
Our interactive dashboards are a central component of our Quality Management Analytics Engine. They move beyond static reports to give you near real-time visibility into your quality performance, empowering your teams to act decisively and improve outcomes.
Here’s how our dashboards drive results:
- Near Real-Time Gap Closure: Our dashboards provide a unified view of care gaps as they are identified. This allows your teams to see which gaps are open and which have been closed, enabling proactive interventions and efficient follow-up. You can easily drill down into specific member populations or providers to prioritize outreach and close gaps faster.
- Targeted Member and Provider Identification: The dashboards make it simple to identify at-risk members who need immediate attention and pinpoint top-performing or under-performing providers within your network. This allows you to deploy resources effectively, focusing on areas that will have the biggest impact on quality scores and member health.
- Actionable STARs Reporting: We go beyond just displaying data. Our dashboards provide a clear, real-time look at your STARs performance, including progress toward key benchmarks and predictive trending for the coming years. You can see how specific measures are trending and where you need to focus to improve your overall rating. This insight helps you strategize and make data-driven decisions that directly impact your financial incentives and competitive position.
The Innovaccer Advantage: A 360° Approach
Innovaccer helps health plans take a comprehensive approach to quality gap closure with prospective, concurrent, and retrospective reviews:
- Prospective Reviews: By analyzing historical data, the platform identifies care gaps early, giving providers ample time to provide preventive care. Combined with our InNote platform, providers are able to bi-directionally document information in their EHRs and the Innovaccer platform to support
- Concurrent Reviews: Monitor care delivery in real-time to ensure open gaps are closed and timely follow-ups are initiated. Concurrent reviews supporting simultaneous clinical and quality abstraction and risk adjustment coding.
- Retrospective Reviews: Analyze past claims and clinical documentation to detect missed interventions, support audits, and improve future reporting. Bi-directional reviews assistance from coding AI copilot.
Chart Retrieval and Abstraction Platform
Innovaccer’s chart retrieval & abstraction platform eliminates the hassle of chasing charts and ensures you always have the right information. It helps health plans capture accurate and compliant data more efficiently by:
- Pulling Charts Directly from EHRs: The system integrates with existing EHRs to automatically retrieve charts, saving significant time and manual effort.
- Reduce Redundant Requests: Innovaccer’s platform allows a single chart retrieved to serve multiple purposes, from HEDIS abstraction to risk adjustment, to reduce the administrative burden and costs around retrieval. The platform includes a retrieval agent that can handle large volume chart requests, which validates if the chart is already within the platform prior to requesting, to reduce duplicate requests. The retrieval agent also handles special requests or attestations, while the platform allows manual management for specific medical requests, ensuring all needs are met efficiently.
- Enabling Real-Time Abstraction: Review and act on documentation gaps across quality programs as they happen, not weeks or months later. Abstraction with NLP-identified support and AI copilot abstraction assistance.
- Closing Gaps from All Angles: Innovaccer’s platform unifies data from payers, providers, pharmacies, and in-home interventions to create a unified patient view. This helps close both risk and quality gaps and enables one-click campaigns for things like medication adherence, at-home test kit ordering, and STARS multi-measure initiatives.
Also read: 360° Gap Closure- The Ultimate Solution to Payers’ Risk and Quality Challenges
The Time to Act is Now
Health plans are at a critical inflection point. In an era of rapid regulatory changes and evolving HEDIS requirements, quality management is more important than ever. Organizations that invest in an integrated, end-to-end approach will be better positioned to respond to changes, close care gaps faster, and provide exceptional member outcomes.
The opportunity is clear: modernize your quality efforts, provide member-first outcomes, and act now.
Ready to see how you can reshape quality management and improve outcomes? Let's connect.

.png)



.png)




