Care Management vs. Case Management: What’s the Real Difference?

Your healthcare organisation operates care management and case management programs. Quick question, what's the difference?
If you paused, you are not alone. These terms are so interchangeable in healthcare that even scholars refer to it as the "black box" problem. When there are no agreed definitions on fundamental terms, technology purchases don’t align with workflows, and care managers are balancing discharge planning while case managers monitor chronic conditions with acute care tools.
The outcome? Expensive chaos masked as coordinated care.
What Is Care Management?
Care management is defined as the proactive, tailored, and long-term coordinated healthcare assistance that monitors and maintains chronically stable patients, preventing costly emergencies.
These patients need someone tracking medication adherence, watching for warning signs, and coordinating between specialists. To ensure proper engagement, care management professionals typically hold only 50 to 100 patients and require real engagement through weekly check-ins, monthly care plan adjustments, and quarterly medication reviews.
Care management programs are designed with the 5% of patients who drive 50% of healthcare costs in mind. Through sustained support, these programs reduce readmissions and emergency visits while improving quality of life.
What Is Case Management?
Case management manages healthcare services during acute medical occurrences like surgeries, strokes, emergency hospitalizations.
In contrast to care management's multi-year relationships, case managers work in crisis mode. They manage 200-300+ cases at one time because each intervention takes days, not months. The job requires quick decisions: Is the patient discharge-ready? Is insurance available for rehabilitation? Who can initiate home health immediately?
Care Management vs. Case Management: Key Differences

Case Manager vs Care Manager: Roles, Teams, and Certifications
Although both work on care coordination, their job requires different skills, certifications, and day-to-day workflows.
Care managers draw long-term relationships with patients having chronic diseases. They mostly possess nursing degrees (RN, BSN) or social work education (MSW), supplemented by specialized care management certifications (CCM) or chronic disease management certifications. Their success relies on relationship-building competencies along with extensive chronic disease knowledge.
Case managers navigate the intricacies of acute care. Similar educational processes equip them to handle various challenges: utilization review, discharge planning, and insurance authorization skill sets. Problem-solving characterizes their role.
When to Use Care Management vs. Case Management
Both methods are necessary in most healthcare systems. Utilize them strategically depending on patient need and organizational objectives.
Care Management
Implement care management for patients with sustained needs throughout their care continuum. Your most expensive, highest-risk patients who are benefiting from relationship-based care coordination and patient activation.
Ideal patients:
- Multiple chronic illnesses (diabetes, HF, COPD)
- Recurrent hospitalizations or ED utilization
- Juggling 10+ medications per day
- Social determinants of health pertaining to transport, housing, food, etc.
- Post-acute patients who need continued monitoring
The value proposition: lower costs over the long-term through prevention, better medication management, and ongoing patient activation.
💡Related Read:
Want to learn more about care management? The Ultimate Guide to Care Management in Healthcare covers proven strategies for managing chronic conditions, reducing costs, and scaling coordinated care across your entire patient population. [Continue Reading →]
Case Management
Case management excels during defined episodes with clear endpoints. Healthcare providers need intensive coordination compressed into critical windows.
Ideal for:
- Multi-site discharges
- Multidisciplinary complex surgeries
- Workers' compensation cases with timelines
- High-cost claims requiring utilization review
- ED super-utilizers requiring timely resource alignment
The return on investment is avoided readmissions, fewer complications, and managed healthcare costs at risky transitions.
Technology and Care Management Tools and Case Management
Care managers navigate several systems every day. They require real-time access to patient medications, appointment records, lab results, and care deficiencies. They need tools that automatically expose at-risk patients, record interactions without manual data entry, and coordinate among multiple providers.
Case managers also encounter the same complexity in acute events. They should have timely access to prior authorizations, bed status, discharge planning information, and insurance coverage information. They should monitor transitions across care locations, validate handoffs, and avoid readmissions.
Both positions share essential requisites:
- Consolidated patient perspectives from all data sources
- Real-time notifications when patients require intervention
- Automated documentation that records interactions
- Seamless care coordination among care teams
- Predictive analytics to avoid crises
Legacy configurations compel the healthcare team to switch between 5-10 systems, re-keying the same data numerous times, missing vital updates that land in systems they're not actively reviewing.
How Innovaccer Combines Both Care and Case Management Workflows
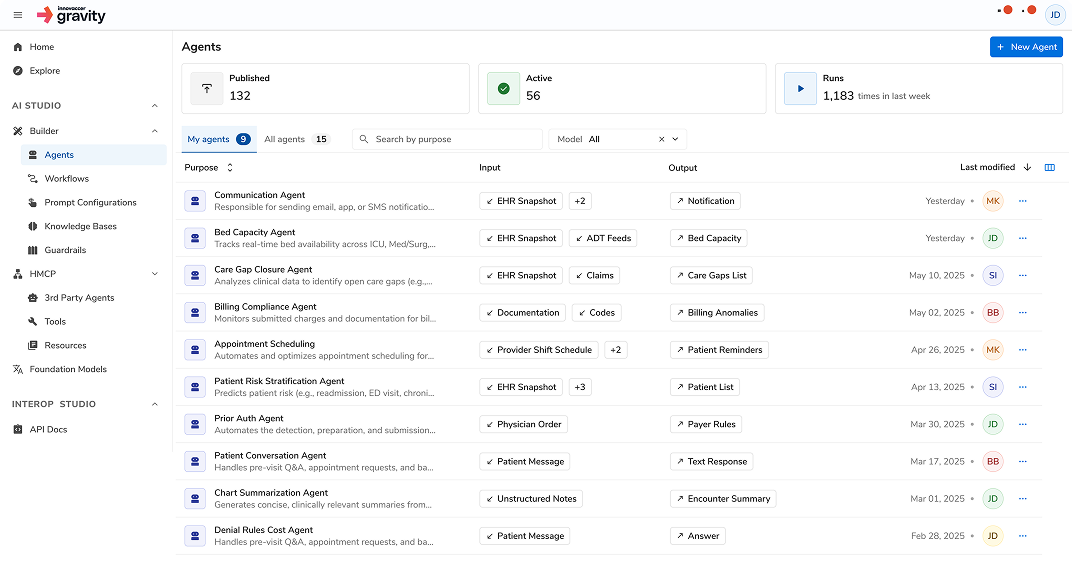
Innovaccer overcomes these obstacles with its Healthcare Intelligence Platform, designed specifically for care coordination. Unlike generic platforms that need to be heavily customized, Innovaccer comes with 10 years of healthcare context pre-installed.
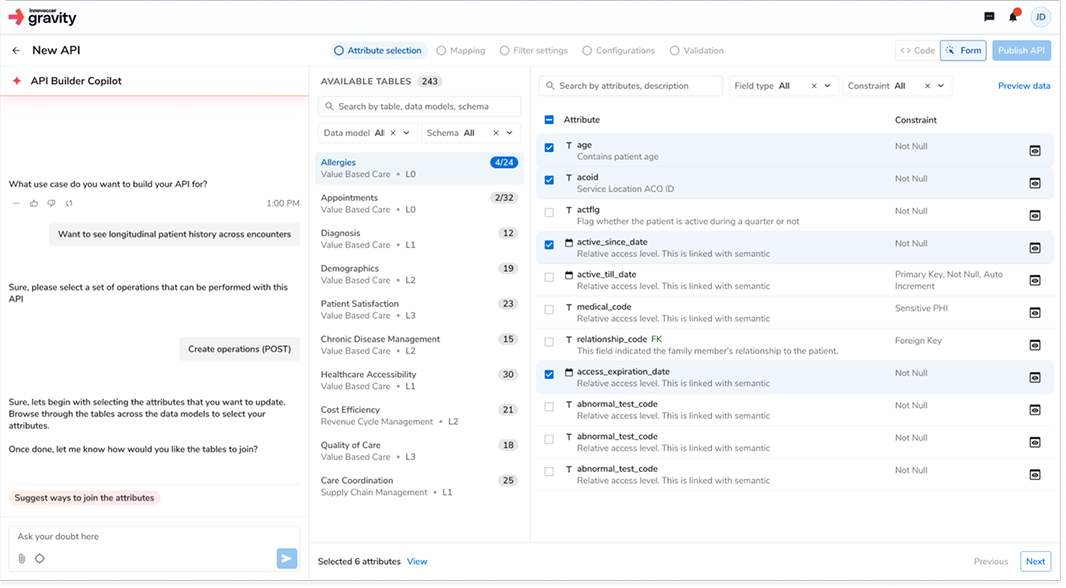
Complete Real-time Data Integration
The Healthcare intelligence Platform automatically integrates clinical, claims, pharmacy, and operational streams of data. When a patient does not show up for an appointment, fills a prescription, or gets treated in an emergency room, both case managers and care managers get notified on their unified dashboards.
Imagine a fictional patient, Jennifer Martinez, with diabetes and hypertension. Her care manager views it all in one place: A1C trends from the lab systems, medication refill rates from the pharmacy claims, appointment history from the scheduling systems, and social determinants from community resources. No signing in to multiple portals. No waiting for batched updates. It all syncs in real time.
Healthcare-native Interoperability
Innovaccer comes with native support for 200+ EMRs and 60+ payers. The platform aligns with the language of healthcare via native HL7, FHIR, and X12 standards support. Its Healthcare Model Context Protocol (HMCP) allows AI agents to function within established clinical workflows.
This equates to when Jennifer's case manager must organize post-discharge services, Innovaccer retrieves her insurance eligibility, available network providers, and prior authorization needed into one workflow automatically. The Pre-built Authorization Agent provides direct requests through payer portals while the care manager continues talking to Jennifer.
AI That Captures and Documents Automatically
Innovaccer's AI Copilots remove documentation drudgery completely. While on phone calls with patients, the system listens, captures essential information, and fills out EHRs automatically. The AI recognizes medical context and provides follow-up suggestions.
Care Management Copilot does the following specifically:
- Transcribes conversations
- Pulls clinical insights and suggests action items
- Updates care plans automatically
- Schedules follow-up activities
- Highlights urgent issues for immediate resolution
Care managers have saved 2-3 hours a day on documentation alone. That's time regained for real patient care.
The Bottom Line: Why Clarity Matters
When organizations don't know the difference between care and case management, they purchase incorrect technology, employ incorrect people, and measure incorrect outcomes.
Clear definitions lead to clear outcomes. Care management avoids crises through ongoing relationships. Case management manages crises through intensive coordination. Both are necessary. Neither replaces the other.
The way forward: Define your terms. Use the appropriate model for the right patients. Invest in integrated technology like Innovaccer that accommodates both workflows without requiring compromises. Provide teams with tools to thrive in their real jobs, not ones in the translation loss.
Because when everyone finally gets on the same page about what care management and case management actually are, something amazing occurs: they begin working together.

.png)



.png)




